Collaboratives – key change agents?
Many of you will be familiar with our Enhancing Quality and Recovery (EQR) programmes. They provide clinical teams with an effective methodology for service improvement based on a collaborative approach. The evidence suggests they’ve been very successful across Kent, Surrey and Sussex at embedding and spreading best practice which leads to better results for patients.
With that in mind, I’d like to draw your attention to the latest publication from the Health Foundation, Improvement collaboratives in health care. It’s an evidence scan which compiles research about whether quality improvement collaboratives are effective. There’s increasing interest in the health and social care sectors about the potential for collaboratives to be powerful change agents so it’s a very timely document. It looks at the effectiveness of collaboratives in improving healthcare and the impact of other factors.
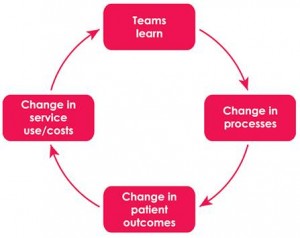
How collaboratives work
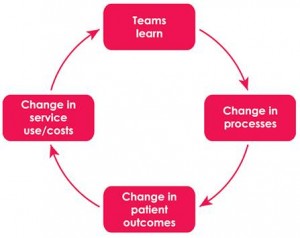
Learn, change, repeat
Although there are a number of different models, collaboratives usually involve teams from across an organisation or a number of organisations working together to achieve agreed outcomes. Sharing learning is integral to the process of spreading best practice and sustaining improvements. In KSS, our EQR collaboratives focus on pathways such as heart failure, acute kidney injury, pneumonia, fractured neck of femur, and dementia. It’s also the approach behind the new Patient Safety Collaborative which is due to launch in the autumn.
We are fortunate that the EQR methodology is well established in KSS and able to demonstrate sustained improvements across a number of pathways. The Health Foundation concludes that “collaboratives may have some potential to support improvements in the quality of health care but, like most initiatives, they are not a ‘silver bullet’ and cannot be relied upon in isolation to spread broad change”. The report also highlights the likely characteristics of successful collaborative include:
- well facilitated programme management
- the value assigned by the organisation and teams to the collaborative methodology
- the length of data collection
- perceived support from junior doctors
- inter-professional collaboration
- organisational readiness
They will resonate I’m sure with colleagues who have been involved with EQR. It’s encouraging to see key components of the KSS EQR programmes on a list generated by participants in the Health Foundation’s research. Our role is to create the environment in which collaboration can flourish; it’s the clinical teams, committed to a collaborative approach, sharing data and learning, who translate the methodology into better outcomes for patients. The report notes that sustainability can be an issue for improvement – whether delivered through a collaborative approach or not – and this is something built into the EQR approach. Annually agreed targets and ongoing data measurement ensure momentum for continuous improvement and reduce variations in the quality of care across KSS.
If you’d like to know more about EQR, please get in touch with Kay Mackay, our Director of Improvement, via kay.mackay1@nhs.net
Kind regards,
Guy Boersma
Managing Director, KSS AHSN
KSS AHSN Commercial Director job vacancy
KSS AHSN is at an exciting stage in our development, as we look to grow our team to include a Commercial Director.
Our Commercial Director will drive forward our ambitions and help to shape our business model, using stakeholder and market input to ensure we develop compelling membership and service offerings that are commercially sustainable and focus on positive patient outcomes.
For full details on the role and how to apply for the position, please download the candidate appointment briefing document here.
Health Innovation Challenge Fund
The Health Innovation Challenge Fund invites applicants to apply for funding in any of the areas of special interest listed below. Please read the eligibility criteria thoroughly before applying.
Each £10m funding round will review and assess proposals from all themes. All applications are judged purely on merit. There are no funding quotas for individual themes.
For further information and details, please click here.
Opportunity to Get Involved in the Systems Leadership, Local Vision Programme
The Local Government Authority led, Systems Leadership Steering Group is looking for applications for the second round of Systems Leadership – Local Vision projects across the country. The projects bring people together from across the NHS, public health, local government, social care and other services, in order to create new ways of working on ‘wicked’ issues and achieve measurable improvements in health, care and wellbeing.
Read more here
Horizon 2020 – Launch of 2015 Calls
The revised versions of the Horizon 2020 work programmes have been adopted and uploaded onto the Horizon 2020 website. The revised version of the Health, Demographic Change and Wellbeing work programme can be accessed here.
The call for the 2015 topics opened on 30 July 2014. You can see the calls for proposals online, on the Horizon 2020 calls for proposals portal.
Nutrition and Hydration Week 16 – 22 March 2015: A Global Challenge
2015 will see the 4th Nutrition and Hydration Week.
For further information about plans for 2015 and activities this year please click here.