In this week’s edition:
Towards the end of last week the King’s Fund published A new settlement for health and social care. It’s the final report of the independent Commission on the Future of Health and Social Care in England chaired by Kate Barker. It’s different to another commission – the one led by Sir John Oldham on which Marion Dinwoodie from Kent Community Health NHS Trust participated in and which I wrote about recently.
The Barker commission focuses particularly on the funding challenges facing the government arising from the growing and ageing population, rising rates of long-term conditions and increasingly expensive treatments.
It finds that if the government does nothing “fewer people will receive publicly funded social care as further cuts are made to local authority budgets and more NHS organisations find themselves unable to provide timely access to acceptable standards of care within budget.”
People needing access to care will also be forced to continue to navigate the complexities and inconsistencies of the current fragmented systems of funding and entitlement. To quote the report, “the costs of this care will fall increasingly to individuals and families, creating worry, uncertainty and inequity on a scale that would be unacceptable.”
Complexity
We often refer to the complexity and confusion surrounding current provision of services. The Barker report highlights the difficulties for patients, carers and families in navigating the complexities of health and social care finances.
It sets out proposals to introduce a simpler path for the public to navigate through the current maze of cash benefits, and health and social care funding. Its major recommendation is integrated health and social care commissioning.
I’m sure that between now and the general election there will be further reports and policy proposals about future funding for health and social care; this one is well worth a read.
KSS EXPO and awards
This will be a major event for the region and an outstanding opportunity for new collaborations to begin and for innovation to spread. It takes place in London on 13 January 2015.
Registration will open shortly and by way of appetiser, I’d like to share with you the thoughts of some attendees at our Partnership Day earlier in the summer – which also gives me the chance to publicly thank everyone who agreed to be interviewed in our new video; thank you!
Kind regards,
Guy Boersma
Managing Director, KSS AHSN
***
Kent Surrey Sussex Patient Safety Collaborative Bulletin
The third edition of the Kent Surrey Sussex Patient Safety Collaborative (KSS PSC) Bulletin was published last month. Through these bulletins the KSS PSC aims to keep you informed about developments regarding the new KSS PSC. You can access the bulletin here: KSS PSC Bulletin 3 – August 2014
The Sir Jules Thorn Award for Biomedical Research
[The Sir Jules Thorn Trust]
One grant of up to £1.5 million is offered annually to support a five-year programme of translational biomedical research selected following a competition among applicants sponsored by the leading UK medical schools and NHS organisations.
UK medical schools and NHS organisations are eligible to submit one application annually.
Prospective applicants should note that:
- The closing date for Preliminary Applications is 3 October 2014
- Only one application per institution is permitted
- The Award may not be used for Cancer or HIV/AIDS related research.
For more details, please click here.
NHS and PHE South Region’s sustainability conference: Putting Sustainability into Practice
[The South Regional Network (SRN)]
Where: Reading Town Hall, Blagrave Street, Reading RG1 1QH
When: 10.00 – 16.00 on Wednesday 1 October 2014
The overall aim of this event is to share good practice and inspire us to new more sustainable ways of working and living.
The day will include participative workshops on the topics below:
- Adaptation and Resilience
- JSNA – sustainability chapter
- Pharmaceuticals and Medicines – green bags, inhaler recycling
- Optimising Social Value
- Commissioning and Procurement
- Active Transport
- Sustainable Carbon Emissions – measurement and modelling of carbon for providers and commissioners
- Health Co-benefits – making it real
To apply, please click here or email Georgina Dove: georginadove@nhs.net
NHS patients could benefit from new models of care used around the world
[Monitor]
The health sector regulator is looking into how important acute services are provided by hospitals in other countries including France, Germany, Canada and America to see what lessons the NHS can learn.
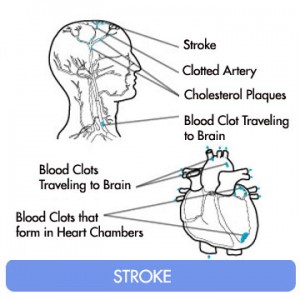
Monitor will examine how other countries set clinical standards and set out to achieve good quality care in a range of services including stroke, maternity, and A&E.
The analysis will lead to examples of models of care which can be adapted by the NHS to deliver equivalent or better services more efficiently.
Read the full press release here.
Research scan alert
[The Health Foundation]
August’s research scan alert from the Health Foundation featured highlights of the latest studies about healthcare improvement. Focusing on studies in four areas:
- Person-centred care
- Patient safety
- Value for money
- Approaches to improvement.
Read the selection of highlighted articles, here.
Update on Urgent and Emergency Care Review
[NHS England]
NHS England has published an update on the Urgent and Emergency Care Review, which builds on NHS England’s future vision for urgent and emergency care in Transforming urgent and emergency care services in England. Urgent and Emergency Care Review End of Phase 1 Report. This work will make it easier for patients to get the right care, in the right place, first time.
For more information, please click here.