By Martin Michaelis and Mark Wass. The rapid development of COVID-19 vaccines has been enabled by decades of research, and it could have all gone wrong.
The development of COVID-19 vaccines happened at an unprecedented speed. This was enabled by three main factors. 1) Vaccine platforms were already available that could readily be adapted to COVID-19. 2) There was a preparedness to invest into the production of hundreds of millions of vaccine doses before it was known whether they would be effective. 3) The pandemic provided many willing participants for clinical trials.
Most importantly, decades of progress have resulted in the availability of universal vaccine platforms that can be quickly adapted to new pathogens in a process that resembles changing the tyres on a car. Currently, so-called adenoviral vector vaccines (Oxford/ AstraZeneca) and mRNA vaccines (BioNTech/ Pfizer, Moderna) are used in the UK. These vaccine types can be produced without cultivating the respective pathogen. Therefore, scientists were able to start designing vaccine candidates as soon as the genomic sequence of SARS-CoV-2, the coronavirus that causes COVID-19, became available in January 2020.
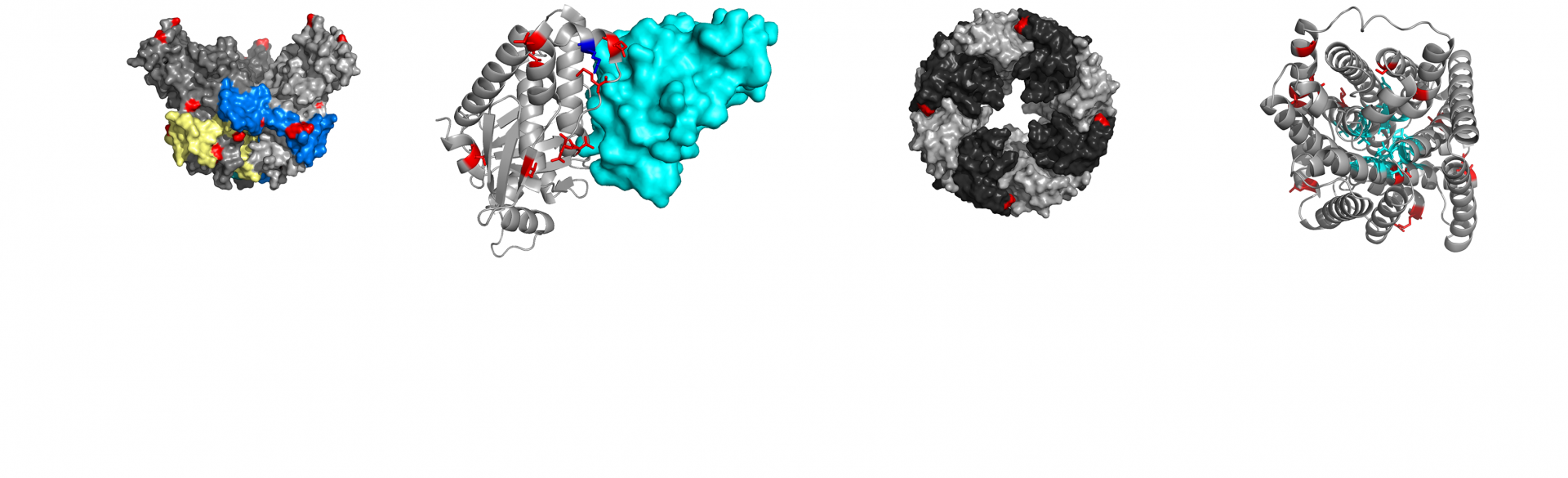
Vector-based vaccines are one of these platforms. They use the inherent capacity of viruses to infect and reprogramme cells. Once the machinery required for virus replication is removed, a virus becomes a vector that cannot replicate anymore but can still infect cells and makes them produce a desired protein. Many vectors, such as the Oxford/ AstraZeneca vaccine (ChAdOx1) vaccine, are based on adenoviruses, because adenoviruses can infect many different cell types. Adenoviral vectors were first used in humans in 1992.
However, some adenoviruses cause common cold-like diseases in humans. Hence, people who have been in contact with a adenovirus used as a vector may have immunity that prevents the vaccine from working. To avoid this, vectors are based on exotic adenoviruses with whom humans have not been previously in contact, such as the Chimpanzee adenovirus vector in the Oxford/ AstraZeneca vaccine. Since adenoviral vectors represent a very versatile vaccine platforms, adenoviral vector vaccines are under development for many diseases. For example, an adenovirus 26-based vector vaccine is approved for the prevention of Ebola virus disease.
Another important vaccine platform is based on the use of messenger RNA (mRNA), the molecules that carry the information needed for cells to synthesise proteins. The proof-of-concept for mRNA vaccines was provided in 1990, but many technical issues and details had to be overcome before the first mRNA vaccine entered clinical trials in 2015. Main issues included a lack of mRNA stability and limited protein production in host cells. However, this method now enables the development of novel vaccines at breathtaking speed. The Moderna mRNA-1273 vaccine was ready for clinical testing 42 days after the genomic sequence of SARS-CoV-2 had become available. The BioNTech/ Pfizer COVID-19 vaccine (BNT162b2) was the first vaccine for which clinical trial results were reported.
Due to the availability of such universal vaccine platforms, it is now possible to develop vaccine candidates in a very short time. However, only some of these vaccine candidates protect us from the respective pathogens, and often we do not know why a vaccine candidate is successful or not. This is why, despite many attempts, it has not yet been possible to develop vaccines against pathogens including human immunodeficiency virus (HIV), tuberculosis, respiratory syncytial virus (RSV), cytomegalovirus, herpes simplex virus, and Epstein-Barr virus.
Whether vaccines are effective or not, may depend more on the pathogen than on the vaccine platform used. In agreement, many more vaccine candidates have been shown to protect from COVID-19. In addition to further adenoviral vector and mRNA vaccines, this also includes more traditional approaches, in which inactivated viruses or virus parts are used.
Taken together, the rapid development of COVID-19 vaccines has been made possible by decades of research and the resulting universal vaccine platforms that can readily be adapted to new pathogens even without cultivating them. However, it is still not possible to predict whether a vaccine will prevent a disease before clinical trials have been completed. Therefore, we could have ended up with hundreds of millions of doses of unusable COVID-19 vaccines. Instead, we have been lucky and have multiple highly effective vaccines available to us.