Recently, I have been invited to take part in a workshop on Prediction in Epidemiology and Healthcare. The event has been organised by Jonanthan Fuller and Luis Flores at King’s College London on 20 June 2014.
The topic – prediction in epidemiology and healthcare – is well in the remit of EBM+. Actually, it is precisely one of the things philosophy of medicine, broadly construed, should be looking at. As the various talks made clear, predicting what will happen is not merely or solely solved using some sophisticated statistical models. It requires a lot of work in conceptualising the objects of prediction as well as its tools. More to the point, predictions go well beyond the problem of establishing the efficacy of treatments. Prediction likewise concerns prognosis, health policy and public health. Also, prediction concerns individuals as well as populations. So here lies an interesting connection between phil med and more classic topics in phil sci.
A dynamic and engaged group of speakers took part in the event: Jonathan Fuller (University of Toronto) and Luis Flores (King’s College London), Alex Broadbent (University of Johannesburg), Jacob Stegenga (University of Utah), Elselijn Kingma (University of Southampton), Barbara Osimani (University of Camerino), Maël Lemoine (University of Tours), Jeremy Howick (Oxford University). Many other people attended the event, such as our EBM+ bloggers Brendan Clarke and Phyllis Illari, Donald Gillies, Margherita Benzi (currently visiting UCL), Brian Hurwitz, David Papineau and many more.
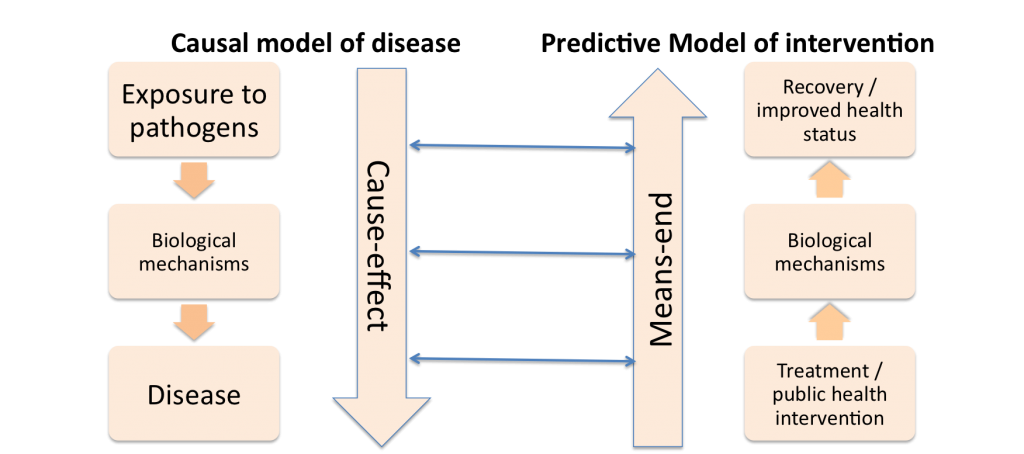
I presented a paper titled “The integration of social and biological mechanisms for healthcare prediction and intervention”. This is work in progress with Mike Kelly, director of NICE, and is a follow up of some previous work on the integration of social, behavioural and biological mechanisms in models of pathogenesis. The idea of the paper is to compare models used for explaining pathogenesis and models to set up interventions. Our point is that the ‘pathogenic model’ has been by and large successful for communicable diseases, as it requires to identify the cause of the disease and to act on it to reduce exposure.
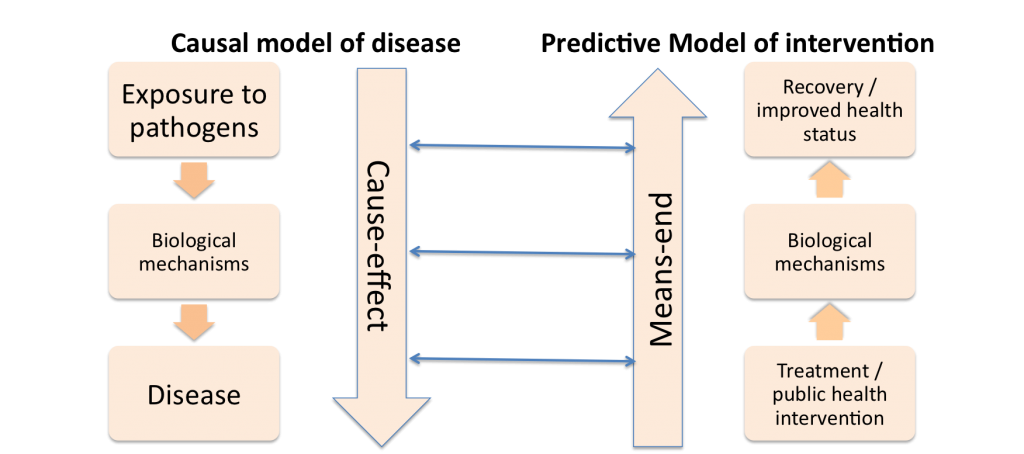
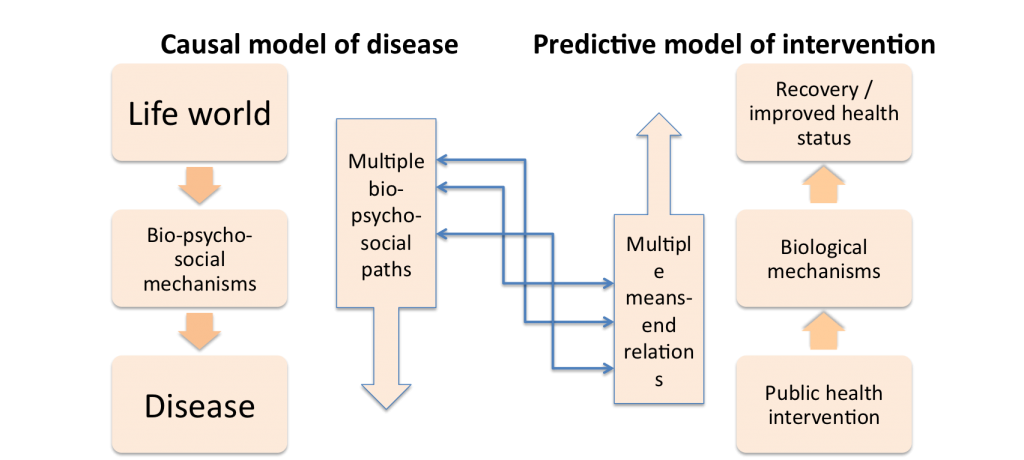
However this model is not as successful in explaining non-communicable diseases, as it neglects mechanisms related to human behaviour. The pathogenic model is even less successful in setting up public health interventions. The reason is that for non-communicable disease (but often for communicable diseases as well) we cannot act on the exposure directly. We instead need to take into account the complex bio-psycho-social mechanisms and we may have to act on indirect factors.
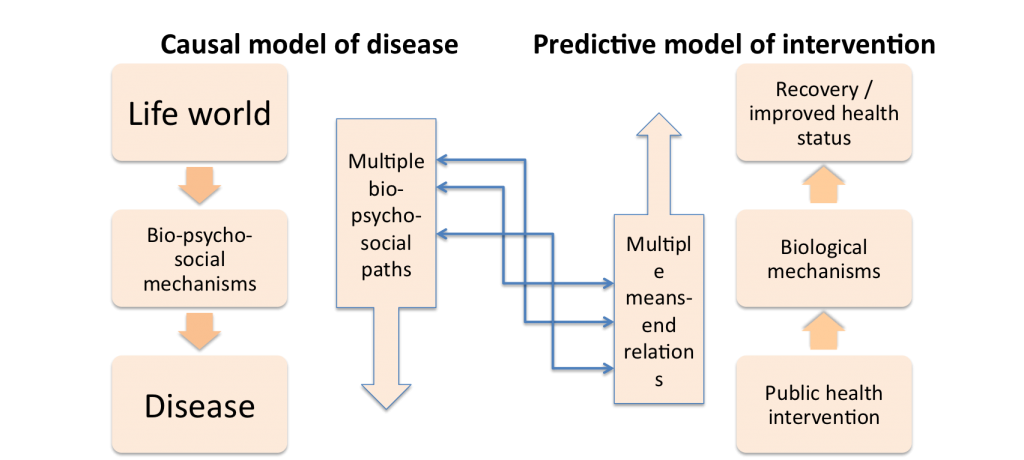
An important point of the paper is precisely the discussion of the integration of the ‘social’ into the biological dimension of disease explanation and prediction.
If you are interested in, here is the presentation: